I have a friend who manages a long list of food allergies — many of the common ones and some less common ones (like pink peppercorn). She also has Oral Allergy Syndrome (OAS) which is also called Pollen Food Syndrome (PFS). (I’ve seen it referred to as ‘Pollen Food Allergy Syndrome’, as well.)
My friend’s mix of severe food allergies plus OAS makes it hard for her to figure out if a symptom like an itchy mouth means a severe allergic reaction is brewing (as in anaphylaxis, as in inject epinephrine, as in head to the ER), or if it’s just OAS from eating a trigger food, and the reaction won’t escalate. Because her food allergy symptoms vary a lot, whenever any symptom appears, this uncertainty about the cause and her history of anaphylaxis make her anxious.
For peace of mind, she finds it easier just to avoid all trigger foods, in addition to all foods she’s allergic to, making for a very {VERY} long list of foods she can’t and/or won’t eat.**
What’s with the itchy mouth and itchy throat that comes and goes?
The most common symptoms are an itchy mouth, itchy lips, and/or an itchy throat, but other symptoms can occur, such as GI tract issues and more rarely, swelling of the throat.
While the prevalence of OAS is not well documented, it’s a condition that can plague people with seasonal allergies. It’s more common in older children, teens and young adults who may have been eating the cross-reactive fruits or vegetables for some time without issues.
What causes OAS? A case of mistaken identity…
Have you ever had hay fever? Exposure to various pollens and immune system sensitization to those pollens is where it all begins.
The common pollen culprits are birch (trees like alder, beech, hazel, hornbeam and oak trees are also in the birch family), grass and ragweed pollens. These pollens trigger an immune system response — think itchy eyes and skin, runny nose, sneezing — when you are allergic to the proteins found in these pollens.
The structure of some of the proteins found in certain fruits and vegetables (and in some spices and nuts) are similar to some of the proteins in birch, grass and ragweed pollens. This structural similarity sometimes causes your body to mistakenly identify those fruits and vegetables as the allergenic pollens, triggering an immune response when you eat them.
What foods can trigger OAS?
Below is a list of food triggers compiled by AAAAI:
OAS Food Triggers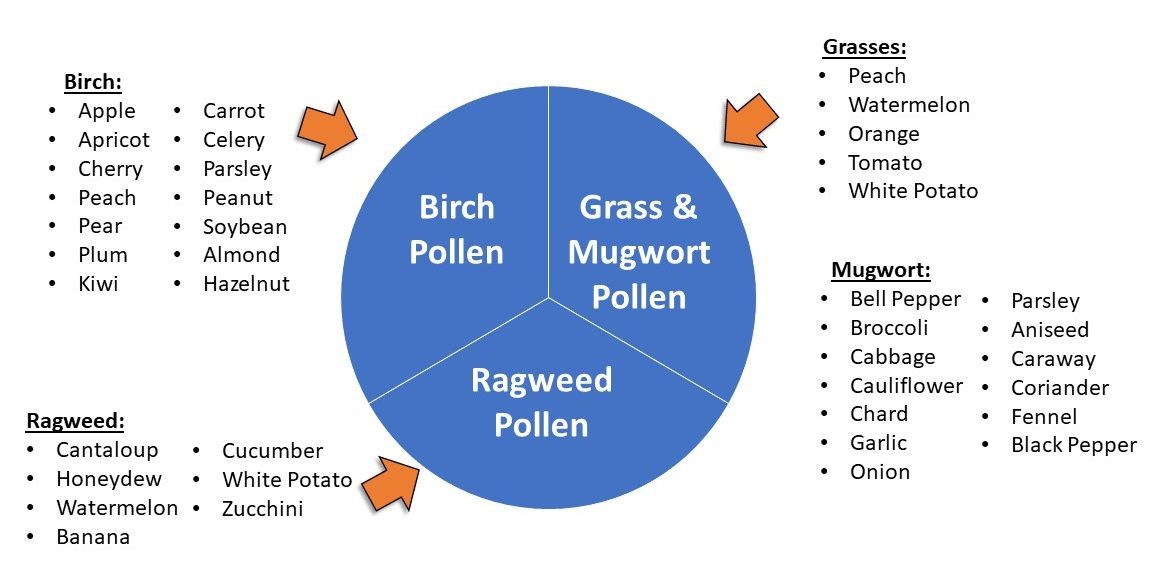
Sources:
- The data in the graphic is from an AAAAI list of food triggers referenced in the Food Allergy Canada webinar.
- Other food trigger lists exist (see the ACAAI resource below*) that vary slightly from the AAAAI-sourced list.
What else should you know about OAS?
Time of year: Symptoms can occur at any time of the year, and sometimes play hide and seek throughout the year, coming and going. Sometimes they may worsen during the cross-reactive pollen season because your body is on high alert from constant bombardment by pollens. Sometimes they may be non-existent at other times of the year.
Individual reactivity: Individual reactivity varies, too. Some people may react to multiple cross- reactive foods. Others may react to just one trigger food, or even to a specific variety of a trigger food (like Granny Smith apples, but not Fuji apples).
Amount sensitivity: Sometimes people can tolerate a little bit of a trigger food, only reacting when they have consumed a larger quantity. Some people only have to peel a trigger fruit or vegetable and they react (proteins are concentrated in the peel which is a plant’s first line of defense in nature.)
Cooked vs. raw: Sometimes people can tolerate a trigger food when it’s cooked (e.g., apple pie vs. raw apples). The heat from the cooking process ‘flattens’ or ‘denatures’ the proteins in the food that mimic the proteins in the pollen — so the antibodies can no longer connect with the fruit & vegetable proteins to trigger an immune response. Sometimes just blanching a food may be enough to break down the proteins. Other times, the food must be very well cooked to be tolerated.
Symptom escalation: In contrast to a food allergy reaction, OAS-related symptoms do not typically escalate to anaphylaxis. According to AAAAI, anaphylaxis from OAS is uncommon.
Herein lies the murkiness….
If you have diagnosed food allergies and OAS, and your mouth and throat start itching after you eat a trigger food, is it OAS? Or, is it the onset of a potentially serious allergic reaction? Will symptoms progress? Or not? The uncertainty can be hugely anxiety-provoking for people with food allergies.
What can you do about OAS?
When you have OAS, you don’t necessarily have to avoid trigger foods if your symptoms are tolerable and don’t make you anxious. However, if symptoms make you extremely uncomfortable or anxious, you may consider completely avoiding all trigger foods.
If the symptoms you experience cause anxiety, you may consider seeking a formal diagnosis from a board-certified allergist. Proper diagnosis can pinpoint your trigger foods with more accuracy so you don’t needlessly avoid foods you might truly enjoy.
How is OAS diagnosed?
Generally, a board-certified allergist would collect data to diagnose your condition and determine the best course of treatment/management for you.
- A detailed history of the symptoms you’ve experienced — exploring the when, where, and how of your reactions. For example, explaining that you are able to eat a cooked version of a fruit or vegetable, but not the raw version, could be a valuable data point for your care provider.
- Skin prick testing could also help identify underlying pollen sensitivities and trigger foods.
- Blood tests might also be ordered as part of the diagnostic process.
- An Oral Food Challenge (OFC) might also be considered. During an OFC, a patient consumes small bites of a suspected trigger food under close medical supervision until a reaction either occurs, or does not.
Helpful resources to learn more
- Food Allergy Canada’s webinar — Understanding OAS/PFAS
- Food Allergy Canada article on OAS + list of trigger foods by pollen category
- The Itch Podcast‘s Episode #42 on — What are cross-reactive allergens?
- AAAAI list of trigger foods by pollen category
- AAAAI article on OAS
- ACAAI article on PFAS
- Asthma & Allergy Network article on OAS
- Article from CHOP (Children’s Hospital of Philadelphia)
 |
Empowering people to live more easily & safely with food allergies through technology & education. |
| About the Author: Gayle Rigione is CEO of Allergy Force, the food allergy management app. She’s also an allergy mom. She’s lived the heart stopping moments when her son ate the wrong thing, second guessed reactions and spent the night in the ER. These experiences inspire her to create tools for people with food allergies. Whatever you do, do it with a full heart. Audentes Fortuna Iuvat | |
Images: Daria Sannikova on Pexels and Allergy Force
**Research Notes
My friend’s story made me curious to learn more about OAS, so I tapped into expert sources to climb the learning curve:
I attended a webinar from Food Allergy Canada. Hosted by Food Allergy Canada’s Executive Director Jennifer Gerdts with Dr. Anne K. Ellis (@DrAnneEllis), Professor and Chair of the Division of Allergy & Immunology in the Department of Medicine at Queen’s University in Ontario. In this webinar — “Understanding Oral Allergy Syndrome / Pollen Food Syndrome” — Dr. Ellis explains OAS in a crystal clear, easy to follow manner. It’s a must watch if you want to know more about OAS.
I also reviewed resources from the American Academy of Asthma Allergy and Immunology (AAAAI), The American College of Allergy, Asthma & Immunology (ACAAI), the Allergy and Asthma Network and Children’s Hospital of Philadelphia (CHOP). *


